【Column Article】Silver World -Lee Bo-Chang’s Column|Earning More but Living Poorly! Why is Taiwan’s Health Faring Worse than South Korea’s?
Although Taiwan’s GDP surpasses South Korea’s, its life expectancy was overtaken by South Korea 20 years ago, and the gap continues to widen. Moreover, the unhealthy life expectancy for Taiwanese people is nearly 8.5 years. The issue lies in a distorted National Health Insurance (NHI) system that indirectly encourages medical institutions to increase outpatient visits while neglecting chronic disease care.
Written by: Lee Bo-Chang
Published: 2024-10-18
When the NHI was introduced in 1995, the average life expectancy for Taiwanese was 74.95 years, compared to 74.15 years in South Korea—Taiwan had nearly a one-year advantage. However, after 2000, South Korea gradually overtook Taiwan in life expectancy. By 2020, Taiwan’s average life expectancy was 81.32 years, while South Korea’s had risen to 83.43 years.
By 2021, South Korea’s average life expectancy exceeded Taiwan’s by 2.7 years, and the gap continues to grow.
Chronic Disease Care is Overlooked under NHI
Overall, Taiwan’s medical standards in fields like medical technology, surgery, and intensive care are on par with developed countries, but its relatively low life expectancy is an undeniable fact. Studies show that Taiwanese people’s healthy life expectancy lags behind that of advanced Western countries, as well as Japan and South Korea. The unhealthy life expectancy of Taiwanese is as high as 8.47 years, a key issue being insufficient public health awareness and inadequate chronic disease care.
At the primary care level, clinics should focus on managing chronic diseases. However, the number of non-chronic disease visits is 4.25 times higher than chronic disease visits. When doctors’ time is occupied by minor conditions like colds and eczema, they have less capacity to adjust medications for chronic patients, making it difficult to reduce the unhealthy life expectancy. This suggests that Taiwan’s medical system is developing abnormally, as chronic diseases—meant to receive proper care—are being ignored. This is a key reason why Taiwan’s life expectancy lags behind countries like Japan and South Korea.
The NHI system, though well-intentioned, aims to provide care for everyone. However, its accessibility is so high, and costs are so low, that it has led to excessive medical consumption, making the situation increasingly difficult to control. This imbalance is also reflected in the distribution of medical resources, with an excessive focus on outpatient care.
Outpatient Overload and the Skewed Focus on Minor Ailments
The heavy burden of outpatient costs stems from the fact that Taiwanese people visit doctors far more frequently than people in Western countries, averaging 15 outpatient visits per person per year. These visits include consultation fees, medication, and various tests (e.g., ultrasounds, X-rays, blood tests), leading to outpatient-related costs accounting for 70% of NHI’s total expenditure, while surgery and hospital stays—critical to saving lives—account for only 30%. In comparison, in advanced countries, the allocation is usually 45% outpatient and 55% inpatient, focusing on life-saving care.
In the case of chronic conditions such as diabetes, hypertension, and high cholesterol, if patients fail to take medication regularly, control their diet, or maintain a healthy weight, these conditions may not lead to immediate organ damage. However, over time, they significantly increase the risk of cardiovascular diseases and death. The challenge for policymakers is to allocate resources wisely, ensuring that NHI focuses on critical care such as severe illness, rare diseases, cancer, and chronic disease management.
Incentives to Maximize Outpatient Visits Limit Time for Chronic Care
There is a clear link between Taiwan’s long unhealthy life expectancy and the quality of chronic disease care. Enhancing the family physician system to ensure all chronic patients receive proper medical care and medication is the goal for the healthcare community and government reform efforts.
With over 5 million hypertension patients and more than 2 million diabetics, managing multiple chronic conditions adds to the challenge. For example, treating diabetes requires not only prescribing medication but also providing dietary education and case management to encourage patients to develop habits of regular follow-up visits and medication adherence. These require time, manpower, and costs that many primary care clinics cannot afford due to their focus on maximizing patient volume.
For years, many medical institutions have adopted a “volume-based” approach, accepting every patient they can. This leads to shorter consultation times, sometimes only a few minutes. For chronic patients, doctors may not have enough time to fully understand their condition, let alone provide adequate education or communication.
Even if chronic patients are diligent about attending follow-up visits, there’s limited time to discuss their health concerns. Many leave the clinic regretting that they didn’t ask the right questions. If patients don’t prepare ahead, it’s easy to miss critical information.
Family Physicians at the Core of Addressing Taiwan’s Life Expectancy Problem
Improving Taiwan’s low life expectancy requires primary care doctors to take a more comprehensive approach to patient care, focusing not on patient volume but on spending sufficient time to treat and manage chronic diseases effectively.
At the “Health Taiwan Forum,” the medical community proposed the “888 Plan,” which President Lai Ching-te endorsed. This plan, targeting chronic patients, aims for 80% of patients with hypertension, diabetes, and hyperlipidemia to be included in the chronic disease management network, 80% of whom will receive lifestyle counseling, with 80% successfully managing their condition within eight years. The “Everybody Doctor Plan” under the NHI will play a crucial role in achieving these goals.
However, whether the “Everybody Doctor Plan” can indeed manage the nearly 6 million chronic patients remains to be seen. Starting in 2024, the long-running “National Health Insurance Family Physician Integrated Care Plan” will evolve into the “Everybody Doctor Plan.” This new plan emphasizes patient-centered holistic care, integrating diabetes, early-stage chronic kidney disease, and metabolic syndrome services, allowing patients to receive comprehensive care from a single medical institution.
Challenges and Future Prospects
While the “Everybody Doctor Plan” aspires to include all chronic patients, achieving this will require not only time but also significant manpower and resources. Furthermore, elderly chronic patients, who form the bulk of this demographic, often face challenges using modern digital tools, making it difficult to gather the necessary data.
In conclusion, whether the Ministry of Health and Welfare’s “Everybody Doctor Plan” can deliver on its promises and improve life expectancy remains a critical issue to watch. If the focus remains on medication with little emphasis on education, real reform will be hard to achieve.
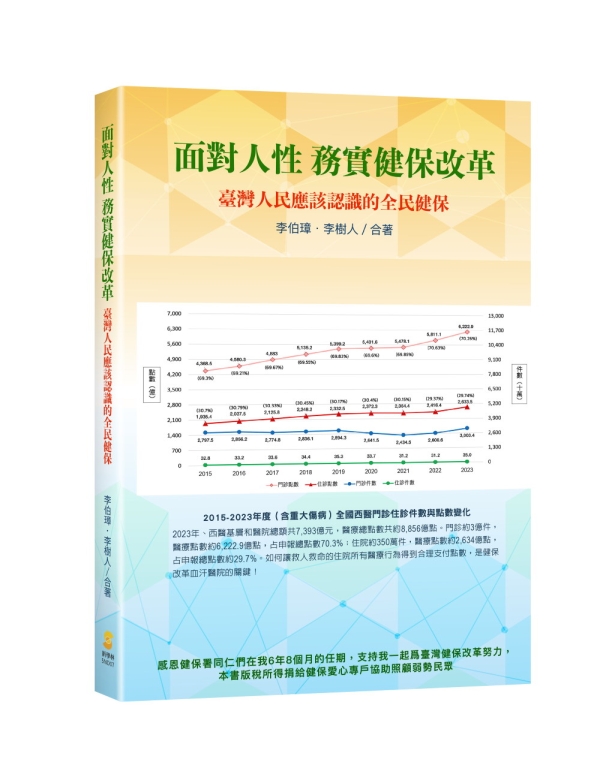
(This article is excerpted from “Facing Human Nature, Pragmatic NHI Reform: What Taiwanese People Should Know About NHI” by Lee Bo-Chang and Lee Shu-Ren, published by New Xue Lin Press)
Original Source: Silver World
Lee Bo-Chang’s Column|Earning More but Living Poorly! Why is Taiwan’s Health Faring Worse than South Korea’s?